Benefits of Shiftwave® Nervous System Regulation

Executive Summary
The Importance of Autonomic Nervous System Balance
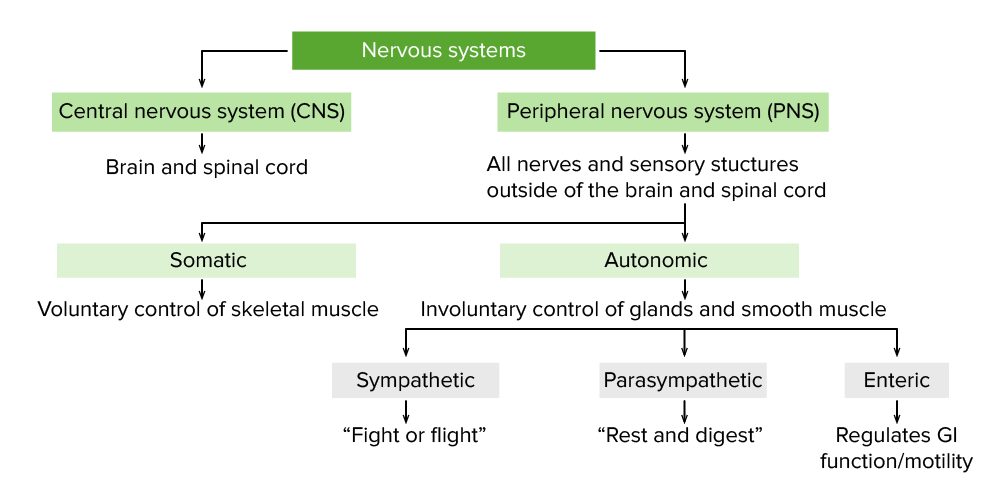
The autonomic nervous system (ANS) plays a fundamental role in regulating involuntary physiological processes such as heart rate, digestion, respiration, and the body’s response to stress. The ANS has two main branches: the sympathetic nervous system (SNS), which drives the body’s "fight-or-flight" responses, and the parasympathetic nervous system (PNS), responsible for "rest-and-digest" functions. Maintaining a healthy balance between these systems is essential for physical and mental well-being. Disruptions in this balance can result in conditions such as chronic stress, anxiety, insomnia, fatigue, and an increased risk of cardiovascular diseases.
How Shiftwave Works
Shiftwave’s Pulsed Pressure Wave™ technology communicates through the body’s natural sense of touch, stimulating mechanoreceptors in the skin, muscles, and organs. Delivered in specific patterns and frequencies, these pressure waves optimize autonomic nervous system (ANS) regulation by modulating both sympathetic (SNS) and parasympathetic (PNS) activity. Precise control of SNS activation increases alertness and energy, while PNS engagement promotes relaxation and recovery, helping to flush stress from your system and build a healthier, more resilient nervous system over time.
Shiftwave’s patented BioDrive® technology is a breakthrough in nervous system regulation, leveraging your body’s Biological Intelligence (BI) to fully optimize nervous system function in real-time. By continuously monitoring physiological signals, such as heart rate, BioDrive® customizes vibratory patterns to align with your body’s current autonomic state. This real-time feedback system ensures an ideal balance between SNS and PNS activity, reducing stress, enhancing focus, alleviating pain, and accelerating recovery. By dynamically adapting to your body’s natural rhythms, Shiftwave promotes long-term well-being and autonomic balance through precise, personalized stimulation.
The combination of BioDrive® and Pulsed Pressure Wave™ technology makes Shiftwave the world’s most advanced nervous system regulation device. By “exercising” your nervous system—alternating between stress activation and recovery—Shiftwave helps flush out stress, strengthen the nervous system, and build greater resilience. This unique synergy enables precise, adaptive modulation of the ANS, delivering unparalleled benefits in stress management, mental clarity, physical recovery, and overall health. Together, these revolutionary technologies set a new standard for optimizing human performance and resilience.

Measuring Shiftwave® Regulation of the Autonomic Nervous System
Shiftwave stimulates sympathetic and parasympathetic nervous system activity by applying scientifically derived Pulsed Pressure Waves to the body. Two key methods for assessing the function and balance of the autonomic nervous system are electrodermal activity (EDA) and heart rate variability (HRV). EDA measures changes in skin conductance, which are directly linked to SNS activation and provide real-time insights into sympathetic arousal (Boucsein, 2012). HRV, the variability in time between heartbeats, reflects the dynamic interaction between the SNS and PNS and is an indicator of overall autonomic flexibility. High HRV is associated with better stress management and resilience, while low HRV is linked to chronic stress and reduced autonomic adaptability (Thayer et al., 2010).
Electrodermal Activity (EDA) as a Measure of Sympathetic Nervous System Activation
Electrodermal activity (EDA) is a widely used measure in psychophysiology to assess sympathetic nervous system (SNS) activation, detecting changes in skin conductance that increase as the SNS activates sweat glands during stress or arousal. This makes EDA an ideal real-time indicator of the body's sympathetic response. With Shiftwave's Pulsed Pressure Waves, modulation of sympathetic activity can be observed directly through changes in EDA, providing real-time feedback on autonomic regulation. These Pulsed Pressure Waves precisely drive sympathetic activity, as evidenced by the increase and decrease in EDA measurements, as seen in the figure below, where EDA rises and falls in response to the activation and deactivation of the SNS. This ability to control SNS activity allows for targeted interventions to regulate stress and physiological arousal, making Shiftwave an effective tool for managing conditions related to sympathetic overactivation, such as anxiety and stress (Critchley, 2002; Boucsein, 2012).
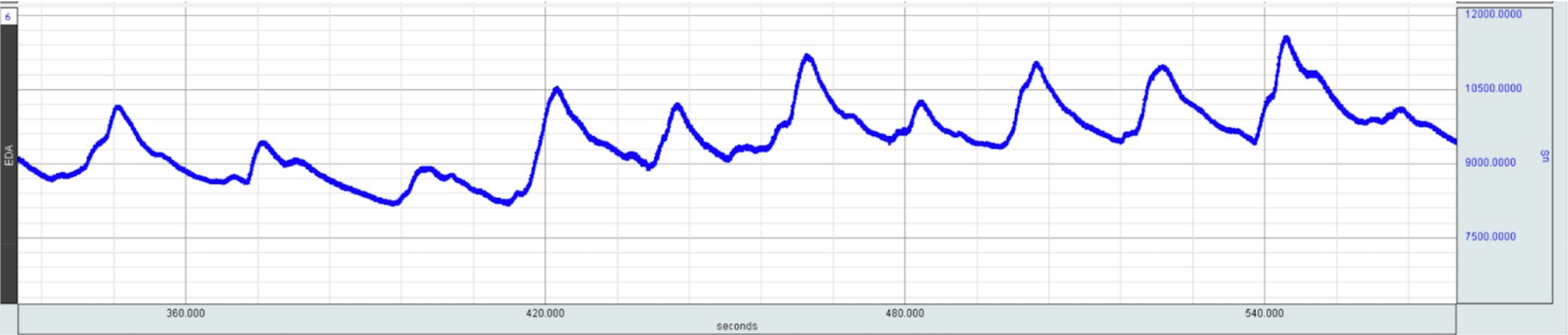
Figure: Electrodermal Activity (EDA) over time illustrates peaks during Pulsed Pressure Wave stimulation, indicating activation of the sympathetic nervous system (SNS), and valleys reflecting SNS deactivation.
Heart Rate Variability (HRV) as a Measure of Autonomic Balance
Heart rate variability (HRV) is a well-recognized measure of autonomic nervous system balance, reflecting the interplay between the sympathetic and parasympathetic branches. HRV measures the time intervals between heartbeats, and a higher HRV indicates a healthy autonomic nervous system with the ability to rapidly switch between SNS and PNS states. High HRV is associated with better cardiovascular health, emotional regulation, and stress resilience, while low HRV often signals chronic stress and poor autonomic flexibility (Thayer et al., 2010).

Figure: Heart rate displaying little periodicity and low HRV.
Shiftwave's Pulsed Pressure Waves are scientifically designed to directly influence the autonomic nervous system (ANS), effectively engaging both the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). These calibrated pressure patterns stimulate the SNS to increase heart rate and activate the PNS to decrease it, thereby providing precise control over autonomic balance. By enhancing both sympathetic and parasympathetic activity, Shiftwave promotes heart rate variability (HRV), which is an indicator of a flexible and adaptable nervous system. Improved HRV reflects better autonomic regulation, aiding users in managing stress responses and enhancing recovery. In the figures below, you can see how Pulsed Pressure Waves drive heart rate up and down, demonstrating Shiftwave's ability to control both SNS and PNS activity, as well as the resulting increase in HRV.
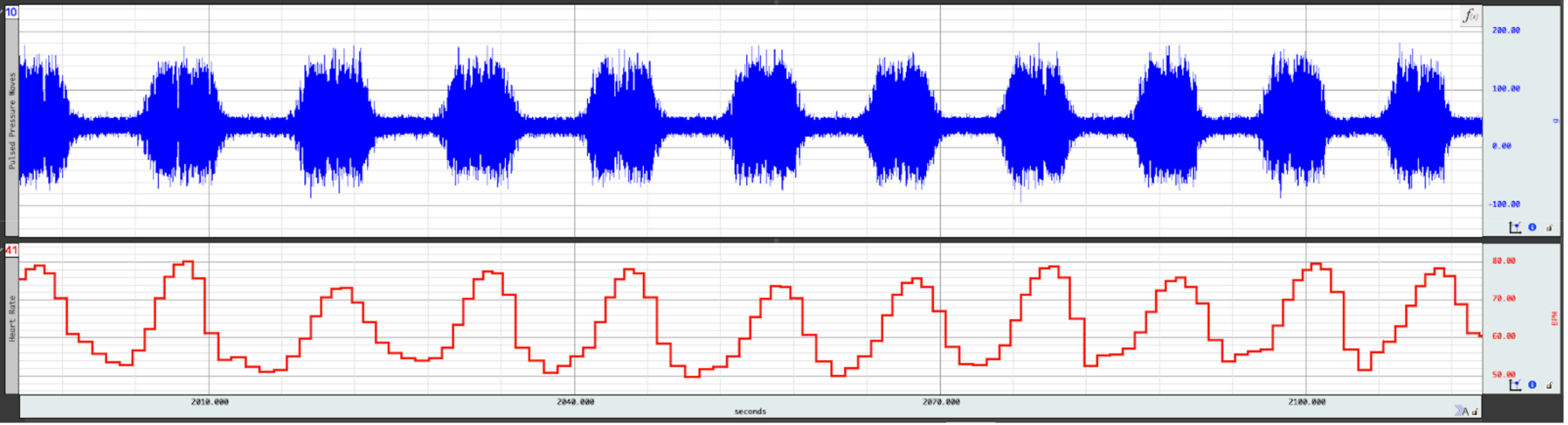
Figure: (Top) Accelerometer data showing complex pulsed pressure waveforms. (Bottom) ECG data showing Pulsed Pressure Waves driving heart rate up and down into optimized periodicity representative of a regulated nervous system.
Heart rate is a valuable indicator of autonomic nervous system (ANS) balance, reflecting the dynamic interplay between the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). When the SNS is activated, it increases heart rate to prepare the body for "fight-or-flight" responses, enhancing alertness and readiness for action. In contrast, PNS activation decreases heart rate, promoting relaxation and recovery through the "rest-and-digest" functions. The degree to which the heart rate fluctuates in response to these opposing forces is known as heart rate variability (HRV). A healthy nervous system exhibits high HRV, meaning the heart can adjust its rate up and down quickly depending on the body's needs. This flexibility signifies a robust ability to respond to stress and return to a calm state. Low HRV, however, indicates a lack of adaptability, often associated with chronic stress, fatigue, or poor health. Therefore, heart rate and its variability offer important insights into the balance and resilience of the autonomic nervous system.

Expanded Explanation of the Benefits of a Regulated Nervous System
1. Sleep
A well-regulated nervous system, particularly the autonomic nervous system (ANS), is essential for healthy sleep patterns. The autonomic nervous system consists of two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). These two systems work together to ensure the body can both wake up and sleep effectively. Here's how a regulated nervous system affects sleep:
Sympathetic Nervous System (SNS) Suppression:
The sympathetic nervous system, responsible for the "fight-or-flight" response, is generally active during waking hours. For proper sleep, this system needs to be suppressed, allowing the body to relax. Overactivity of the SNS, due to stress or anxiety, can lead to sleep disorders like insomnia or fragmented sleep. Suppression of the SNS is critical for entering restful, deep sleep (Lombardi, Pengo, & Parati, 2019).
Parasympathetic Nervous System (PNS) Activation:
The parasympathetic nervous system promotes relaxation and is key to restorative sleep. It slows the heart rate, lowers blood pressure, and reduces muscle tension, all of which are necessary for deep, restorative sleep. Parasympathetic dominance during sleep, especially during non-REM (NREM) stages, supports the body's recovery and healing processes (Kadoya & Koyama, 2019).
Heart Rate Variability (HRV):
A well-regulated nervous system is associated with balanced heart rate variability (HRV), a measure of the variation in time between heartbeats. Higher HRV during sleep is linked to greater parasympathetic activity, signaling more restorative and restful sleep. Conversely, lower HRV may indicate stress or poor sleep quality, often due to an overactive SNS (Meerlo, Sgoifo, & Suchecki, 2008).
Transition Between Sleep Stages:
Proper regulation of the nervous system helps facilitate smooth transitions between the various stages of sleep, including light sleep, deep sleep (slow-wave sleep), and REM sleep. During deep sleep, parasympathetic dominance is essential for bodily restoration. During REM sleep, there is a subtle increase in sympathetic activity related to mental processing and dreaming (Moldofsky & Luk, 2002).
Stress and Sleep Disorders:
A dysregulated nervous system, particularly heightened sympathetic activity, can lead to stress-related sleep disorders such as insomnia or restless leg syndrome. Chronic stress activates the SNS, making it harder for the body to transition into the restful state needed for sleep (Lombardi, Pengo, & Parati, 2019).
Autonomic Regulation of Cerebrospinal Fluid (CSF):
Recent research has shed light on regulating cerebrospinal fluid (CSF) flow and its connection to the autonomic nervous system. Cerebrovascular activity, influenced by autonomic activation, plays a significant role in generating CSF pulsations (Wang et al., 2022). Autonomic arousals contribute to brain fluid pulsations during sleep, suggesting that CSF flow regulation may not solely depend on slow electrocortical activity (Picchioni et al., 2021). The glymphatic system, a brain-wide network of perivascular spaces, facilitates CSF and interstitial fluid exchange, potentially linking brain injury, neuroinflammation, and neurodegeneration (Simon & Iliff, 2016). MRI studies have revealed new pathways regulating CSF production, absorption, and clearance, expanding our understanding of CSF physiology and waste removal (McKnight et al., 2020). These findings highlight the importance of proper autoregulatory control of cerebral blood flow in maintaining brain health and suggest potential therapeutic targets for neurodegenerative, neurovascular, and neuroinflammatory diseases.
Conclusion:
A properly regulated autonomic nervous system helps ensure restful, uninterrupted sleep by balancing sympathetic and parasympathetic activities. This regulation facilitates smooth transitions between sleep stages, promotes deep and restorative sleep, and reduces the likelihood of stress-induced sleep disorders.
2. Stress and Anxiety
A well-regulated autonomic nervous system (ANS) plays a vital role in managing stress levels, influencing how the body reacts to and recovers from stressors. The ANS modulates physiological responses through the sympathetic nervous system (SNS) and parasympathetic nervous system (PNS), which either heighten or alleviate stress responses. Here’s how a balanced nervous system can help mitigate stress:
Sympathetic Nervous System (SNS) Activation and Stress Response:
The SNS is responsible for initiating the body’s “fight-or-flight” response, increasing heart rate, blood pressure, and stress hormone production like cortisol and adrenaline. This response is essential for short-term survival, as it enables the body to react quickly to perceived dangers or stressors. However, chronic overactivation of the SNS—due to prolonged stress—can lead to heightened anxiety, muscle tension, and fatigue. By modulating the SNS, a well-regulated nervous system prevents the excessive release of stress hormones, reducing the long-term effects of stress on both the mind and body (McEwen, 2007).
Parasympathetic Nervous System (PNS) Activation for Stress Recovery:
The PNS, often referred to as the “rest-and-digest” system, counterbalances the SNS by promoting relaxation and recovery. When activated, the PNS lowers heart rate and blood pressure, facilitates digestion, and calms the mind. This state is essential for stress recovery, allowing the body to repair itself after the SNS has been engaged. Regular PNS activation through relaxation techniques or autonomic regulation ensures that the body can return to a calm baseline after stressful situations, reducing the risk of chronic stress (Thayer et al., 2009).
Balancing the Sympathetic and Parasympathetic Systems:
A well-regulated nervous system maintains an optimal balance between SNS and PNS activity, enabling smooth transitions between stress responses and recovery. Chronic stress often disrupts this balance, leading to prolonged SNS activation, which can result in conditions such as anxiety, high blood pressure, and chronic fatigue. Effective stress management requires both the ability to activate the SNS when needed and the capacity to engage the PNS to foster recovery and relaxation (McEwen, 2007).
Impact on Heart Rate Variability (HRV) and Stress Management:
Heart rate variability (HRV) is a key indicator of autonomic balance and overall resilience to stress. High HRV reflects a strong ability to switch between SNS and PNS activity, which is critical for adapting to and recovering from stress. Low HRV, on the other hand, indicates reduced flexibility in managing stress, often associated with anxiety and burnout. A well-regulated nervous system supports high HRV, improving the body’s ability to handle stress efficiently (Thayer et al., 2009).
Stress and Cognitive Function:
Chronic stress impairs the prefrontal cortex, the area of the brain responsible for executive functions such as decision-making, emotional regulation, and attention. When the nervous system is in a prolonged state of sympathetic activation, cognitive flexibility is diminished, leading to reduced problem-solving abilities and increased mental fatigue. By maintaining a balance between SNS and PNS activation, the nervous system preserves cognitive function, allowing for clearer thinking and better emotional control even in stressful situations (Arnsten, 2009).
Conclusion:
A well-regulated nervous system is essential for managing stress, as it allows for appropriate SNS activation during stressful events and timely PNS activation for recovery. This balance reduces the harmful effects of chronic stress on both physical and mental health, enhancing resilience, cognitive function, and overall well-being.
3. Focus
A well-regulated nervous system, particularly the autonomic nervous system (ANS), plays a crucial role in maintaining focus and concentration. The ANS regulates physiological responses that can either enhance or impair focus, depending on whether the sympathetic nervous system (SNS) or parasympathetic nervous system (PNS) is activated. Here’s how a well-regulated nervous system supports focus:
Sympathetic Nervous System (SNS) Activation for Alertness:
The sympathetic nervous system is responsible for the "fight-or-flight" response, which increases alertness, energy levels, and attention. In moderate amounts, SNS activation enhances focus by increasing norepinephrine and dopamine levels in the brain, which are critical for attention and task performance. This response helps you stay alert and attentive when engaging in demanding cognitive tasks.
However, overactivation of the SNS due to stress or anxiety can have the opposite effect, leading to distractions, reduced focus, and difficulties in concentration. A well-regulated SNS ensures that stress hormones are not excessively elevated, enabling sustained attention without overwhelming anxiety or mental fatigue (Arnsten, 2009).
Parasympathetic Nervous System (PNS) Activation for Relaxation and Sustained Focus:
The parasympathetic nervous system promotes relaxation and recovery, counterbalancing the sympathetic "fight-or-flight" response. When the PNS is active, it helps the body conserve energy, lower heart rate, and calm the mind. This state is ideal for sustained focus, as it prevents mental overload and helps maintain attention on the task at hand without being easily distracted.
A well-regulated PNS allows for periods of relaxation between focused work, preventing burnout and cognitive fatigue, which in turn enhances long-term productivity and focus (Thayer et al., 2009).
Balance Between Sympathetic and Parasympathetic Systems:
A well-regulated nervous system maintains a balance between the SNS and PNS. This balance is essential for switching between periods of high alertness (needed for focusing on complex tasks) and relaxation (which helps consolidate information and recharge mental energy). For optimal focus, the SNS should be moderately active to promote alertness, while the PNS should activate during breaks to maintain overall cognitive health and prevent stress-related distractions.
In individuals with chronic stress, this balance is often disrupted, leading to constant sympathetic overactivation (hyperarousal) and a reduced ability to focus or remain calm (McEwen, 2007).
Regulation of Attention and Cognitive Flexibility:
A well-regulated nervous system supports cognitive flexibility, the ability to shift attention between tasks or thoughts without losing focus. Proper functioning of the prefrontal cortex, which is responsible for executive functions like focus and decision-making, depends on balanced levels of norepinephrine and dopamine, regulated by the autonomic nervous system. When the nervous system is well-regulated, it allows for better attention control, enabling individuals to resist distractions and maintain mental clarity (Arnsten, 2009).
Impact on Heart Rate Variability (HRV) and Focus:
Heart rate variability (HRV), an indicator of autonomic balance, is closely linked to focus. High HRV suggests good balance between the SNS and PNS, promoting calm alertness and improved attention. Low HRV, often associated with stress, can lead to cognitive fatigue and difficulties maintaining focus. A well-regulated nervous system promotes higher HRV, which is conducive to maintaining attention and cognitive performance (Thayer et al., 2009).
Conclusion:
A well-regulated nervous system ensures a healthy balance between sympathetic and parasympathetic activity, promoting alertness, relaxation, and sustained attention. This balance prevents distractions caused by stress and anxiety while fostering long-term focus and cognitive flexibility, critical for both short-term tasks and sustained productivity.
4. Energy and Vitality
A well-regulated nervous system plays a vital role in maintaining energy levels and overall vitality. By balancing the activity of the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), the autonomic nervous system (ANS) ensures that energy is used efficiently, while also promoting recovery and regeneration. Here's how a well-regulated nervous system affects energy and vitality:
Sympathetic Nervous System (SNS) Activation for Energy and Alertness:
The sympathetic nervous system is responsible for the body's "fight-or-flight" response, which is essential for activating energy when needed. When the SNS is activated in a regulated manner, it increases adrenaline and norepinephrine levels, which boost energy, mental alertness, and physical readiness. This is particularly important for responding to daily demands, physical exertion, and moments when heightened energy is required.
A properly functioning SNS provides short bursts of energy without overstimulation. In contrast, chronic SNS activation, often triggered by stress, can lead to fatigue, burnout, and a depletion of energy over time (McEwen, 2007).
Parasympathetic Nervous System (PNS) for Rest, Recovery, and Energy Conservation:
The parasympathetic nervous system promotes relaxation and energy conservation by regulating functions such as digestion, cell repair, and immune function. When the PNS is activated, it helps the body recover from physical and mental exertion, supporting long-term vitality. This recovery process is essential for replenishing energy stores, allowing for sustained physical and mental performance.
A well-regulated PNS helps ensure that energy is conserved and restored during rest periods, preventing exhaustion and allowing the body to maintain high levels of energy throughout the day (Thayer et al., 2009).
Energy Balance Between SNS and PNS:
The balance between the sympathetic and parasympathetic systems is crucial for managing energy and vitality. The SNS provides the energy required for action, while the PNS facilitates recovery. When these systems are in balance, energy is expended and restored in a sustainable way. However, when the nervous system is dysregulated—such as when the SNS is chronically overactive—this can lead to constant energy expenditure, leaving the person feeling fatigued, drained, and low on vitality.
Conversely, if the PNS is overactive without enough SNS activation, the person may feel lethargic, unmotivated, and lacking in energy. Thus, a well-regulated nervous system optimizes the balance between energy production (via the SNS) and recovery (via the PNS), resulting in a sense of sustained vitality (McEwen & Wingfield, 2003).
Impact on Physical Vitality and Resilience:
Physical vitality is directly linked to the body's ability to recover from exertion, and a well-regulated nervous system supports this process. The PNS plays a key role in muscle recovery, tissue repair, and metabolic regulation, ensuring that the body bounces back quickly after physical activity. Proper regulation of the PNS also aids in immune function, which is crucial for maintaining long-term health and preventing energy depletion caused by illness or chronic inflammation (Thayer et al., 2009).
A dysregulated nervous system, on the other hand, can lead to chronic stress and poor recovery, depleting physical vitality and causing prolonged fatigue. A well-regulated system ensures that energy expended during physical exertion is effectively replenished, contributing to overall resilience and vitality.
Mental Energy and Cognitive Function:
Mental energy is another area where the nervous system plays a significant role. Proper regulation of the SNS and PNS ensures that mental energy is available when needed for tasks requiring focus, problem-solving, and decision-making. The prefrontal cortex, which governs these cognitive functions, relies on balanced levels of norepinephrine and dopamine, both regulated by the autonomic nervous system.
When the nervous system is well-regulated, it prevents the mental fatigue and brain fog that can result from chronic overactivation of the SNS. This balance promotes clarity of thought and sustained mental energy, contributing to overall vitality (Arnsten, 2009).
Prevention of Energy Drains Due to Stress:
Chronic stress, often caused by a dysregulated nervous system, drains energy and reduces vitality. Continuous activation of the SNS can lead to adrenal fatigue, a condition where the body's stress response system becomes overworked and depleted, resulting in low energy levels, poor concentration, and a general sense of lethargy. A well-regulated nervous system reduces the likelihood of chronic stress, preserving energy and maintaining overall vitality (McEwen, 2007).
Conclusion:
A well-regulated nervous system optimizes both energy production and recovery. It ensures that the body can respond with energy and alertness when needed while also promoting recovery and conservation of energy during rest. This balance prevents fatigue and burnout, supports physical and mental recovery, and sustains overall vitality.
5. Pain and Neuropathy
Nervous system regulation plays a significant role in how the body perceives and manages pain, as well as in the development and progression of neuropathy. The autonomic nervous system (ANS), along with the central nervous system (CNS) and peripheral nervous system (PNS), interacts to modulate pain signals and influence the severity of neuropathy symptoms. Here’s how proper and improper nervous system regulation impacts pain and neuropathy:
Regulation of Pain Perception:
The nervous system, particularly the central nervous system (CNS), regulates pain by processing signals from the peripheral nervous system (PNS). Pain signals from injury or inflammation travel through peripheral nerves to the spinal cord and then to the brain, where they are interpreted as pain. Proper regulation of these signals ensures that pain perception is proportional to the actual physical damage, helping the body respond appropriately to injury.
When the nervous system is dysregulated, it can lead to amplified pain responses, such as in chronic pain conditions. For example, central sensitization occurs when the CNS becomes overly responsive to pain signals, leading to heightened pain sensitivity (allodynia) and pain from stimuli that wouldn’t normally cause pain (hyperalgesia) (Woolf, 2011).
Autonomic Nervous System (ANS) and Pain Modulation:
The autonomic nervous system (ANS), which includes the sympathetic and parasympathetic branches, also influences pain perception. The sympathetic nervous system (SNS) can exacerbate pain through the release of stress hormones like norepinephrine and adrenaline, which heighten pain sensitivity, particularly in cases of chronic pain or neuropathic pain. For instance, overactivity of the SNS can aggravate conditions like complex regional pain syndrome (CRPS), where excessive sympathetic activity leads to severe, persistent pain (Martucci et al., 2019).
Conversely, the parasympathetic nervous system (PNS), which promotes relaxation and healing, helps to dampen pain signals. Vagal nerve stimulation, for instance, has been shown to reduce pain by activating the PNS and inhibiting the release of pro-inflammatory cytokines that can worsen pain (Tracey, 2002).
Neuropathy and Nerve Damage:
Neuropathy refers to damage or dysfunction of the peripheral nerves, which can result in pain, numbness, tingling, or weakness. Proper nervous system regulation is key to preventing or managing neuropathy, as nerve damage often results from dysregulated inflammatory responses, metabolic imbalances (such as in diabetes), or chronic stress.
In conditions like diabetic neuropathy, for example, elevated blood glucose levels cause damage to the peripheral nerves. Dysregulation of the autonomic nervous system can exacerbate neuropathy by increasing inflammation and oxidative stress, leading to worsening nerve damage (Callaghan et al., 2012). Additionally, improper regulation of the sympathetic system can lead to ischemia (reduced blood flow), further damaging peripheral nerves.
Sympathetic Nervous System's Role in Neuropathic Pain:
The sympathetic nervous system (SNS) can contribute to neuropathic pain, a type of pain caused by nerve damage or dysfunction. In some cases, the SNS becomes hyperactive, causing the release of norepinephrine at nerve terminals. This excess norepinephrine can sensitize nerves and increase the perception of pain, contributing to the burning, tingling, or shooting pain typical of neuropathy.
Conditions like sympathetically maintained pain (SMP) are a direct result of this process, where the sympathetic nervous system becomes entangled with pain pathways, maintaining pain long after the original injury or cause of nerve damage has healed (Baron, 2006).
Inflammation, Pain, and Neuropathy:
Nervous system dysregulation can increase pro-inflammatory cytokine production, which worsens pain and contributes to nerve damage in neuropathy. Chronic inflammation from immune system dysregulation can damage peripheral nerves, resulting in painful neuropathy. The central nervous system also plays a role here by promoting the release of neuroinflammatory mediators, which sensitize pain pathways and contribute to neuropathic pain (Ji et al., 2014).
A regulated nervous system, on the other hand, can mitigate inflammation through anti-inflammatory reflexes activated by the parasympathetic nervous system. This helps protect against excessive nerve damage and reduces the overall intensity of pain experienced.
Chronic Stress and Pain Sensitization:
Chronic stress, which often results in overactivation of the sympathetic nervous system, is a significant factor in both pain perception and the development of neuropathy. Stress hormones like cortisol and norepinephrine can heighten pain sensitivity, and prolonged exposure to these hormones can damage peripheral nerves. This is one reason why stress management techniques, such as mindfulness or relaxation practices, can help alleviate chronic pain and slow the progression of neuropathy (McEwen, 2007).
Conclusion:
A well-regulated nervous system is crucial for modulating pain and preventing the progression of neuropathy. The sympathetic and parasympathetic branches of the autonomic nervous system interact to balance pain responses, while the central nervous system processes pain signals. Dysregulation of the nervous system can amplify pain perception, contribute to chronic pain conditions, and exacerbate neuropathic pain by increasing inflammation and stress responses.
6. Physical and Mental Recovery
Nervous system regulation plays a critical role in both mental and physical recovery by balancing the activity of the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS) within the autonomic nervous system (ANS). Proper regulation ensures that the body can respond to stressors, recover efficiently, and maintain long-term health and well-being. Here’s how nervous system regulation influences recovery:
Sympathetic Nervous System (SNS) and Acute Stress Response:
The sympathetic nervous system is responsible for the "fight-or-flight" response, which prepares the body to deal with immediate stressors. This involves the release of adrenaline and cortisol, increasing heart rate, blood pressure, and energy availability to meet physical and mental challenges. In the short term, this response is beneficial for coping with stress or physical exertion, such as during exercise or an acute mental challenge.
However, chronic overactivation of the SNS, such as through persistent stress, leads to fatigue, impaired recovery, and the depletion of energy reserves. Continuous stress can negatively impact both physical and mental recovery by reducing the ability to return to a balanced, relaxed state after a stressor (McEwen, 2007).
Parasympathetic Nervous System (PNS) and Restorative Processes:
The parasympathetic nervous system (PNS) is crucial for recovery. When the PNS is active, the body shifts into a state that promotes relaxation, healing, and energy conservation. This is essential for:
- Physical recovery: The PNS enhances processes like muscle repair, cell regeneration, immune function, and digestion. After physical exertion, PNS activity helps reduce inflammation, repair muscle tissue, and replenish energy stores.
- Mental recovery: The PNS also reduces stress hormone levels, lowers heart rate, and calms the mind, which is crucial for cognitive recovery, emotional regulation, and improved focus. It helps prevent mental fatigue and burnout by promoting rest and relaxation (Porges, 2011).
Proper regulation between SNS and PNS ensures that after periods of physical exertion or mental stress, the body can enter a recovery phase, allowing it to rebuild strength and restore mental clarity.
Heart Rate Variability (HRV) as a Recovery Indicator:
Heart rate variability (HRV), the variation in time between heartbeats, is a key indicator of autonomic nervous system balance and recovery. High HRV is associated with good balance between the sympathetic and parasympathetic systems and is considered a marker of the body's ability to efficiently switch between states of stress and recovery.
- Physical recovery: High HRV is linked to faster physical recovery after exercise or injury, as it reflects the dominance of the PNS, which is necessary for tissue repair, reducing inflammation, and replenishing energy reserves.
- Mental recovery: High HRV is also associated with better emotional regulation and mental resilience, suggesting that the nervous system can efficiently recover from mental or emotional stress (Thayer et al., 2009).
Conversely, low HRV is often a sign of chronic stress, overtraining, or insufficient recovery, indicating that the nervous system is struggling to regulate properly and shift from sympathetic activation to parasympathetic recovery.
Stress, Inflammation, and Recovery:
Chronic stress and poor nervous system regulation can lead to elevated cortisol levels and prolonged sympathetic activity, which impairs both physical and mental recovery. High levels of cortisol can contribute to chronic inflammation, which slows tissue repair and can lead to conditions such as overtraining syndrome or burnout.
- Physical recovery: Inadequate nervous system regulation impairs the body's ability to repair muscles, recover energy, and reduce inflammation after physical stress. This can lead to muscle fatigue, delayed recovery, and increased susceptibility to injury.
Mental recovery: Elevated stress hormones and sympathetic overactivation can impair mental recovery, leading to sleep disturbances, mood disorders, and cognitive fatigue. Without proper parasympathetic activation, the brain is less able to reset and recover from cognitive tasks or emotional stress (Sapolsky et al., 2000).
Impact on Sleep and Recovery:
Sleep is one of the most important processes for both mental and physical recovery, and it is heavily influenced by nervous system regulation. During sleep, particularly deep non-REM (NREM) sleep, parasympathetic activity is dominant, allowing for physical recovery processes like muscle repair, tissue growth, and immune system functioning. Inadequate sleep or poor sleep quality, often caused by nervous system dysregulation, can severely impair recovery.
- Mental recovery: Sleep is essential for processing information, consolidating memories, and emotional regulation. During REM sleep, the brain processes emotional experiences and repairs neural connections, which is critical for mental recovery and cognitive function (Walker, 2017).
Physical recovery: Physical recovery during sleep is driven by parasympathetic activation, which reduces stress hormones, lowers heart rate, and enhances muscle repair. Disruptions to sleep, especially when the SNS remains overactive, can delay physical recovery and lead to chronic fatigue.
Vagal Tone and Recovery:
Vagal tone, the activity of the vagus nerve, reflects parasympathetic nervous system activity. High vagal tone is associated with faster recovery, both physically and mentally. The vagus nerve helps regulate inflammation, heart rate, and digestion, all of which are key components of recovery.
- Mental health: High vagal tone is linked to better emotional regulation, improved mood, and reduced anxiety, all of which are crucial for mental recovery after stress.
Physical health: High vagal tone supports efficient physical recovery by enhancing immune function and reducing stress-related inflammation (Porges, 2011).
Conclusion:
The regulation of the nervous system is essential for effective mental and physical recovery. A well-regulated autonomic nervous system, particularly the balance between sympathetic and parasympathetic activity, ensures that the body can respond to stress appropriately and return to a state of rest and healing. The parasympathetic nervous system promotes tissue repair, reduces inflammation, and restores mental clarity, while the sympathetic system provides the energy needed for acute stress responses. Chronic stress and dysregulation, on the other hand, impair recovery, leading to fatigue, slower healing, and mental exhaustion.
7. Longevity
A well-regulated nervous system, especially within the autonomic nervous system (ANS), plays a critical role in promoting longevity by maintaining a balance between stress responses and restorative processes. Longevity is closely tied to the body’s ability to manage stress, reduce inflammation, maintain cellular health, and support overall physical and mental well-being, all of which are deeply influenced by nervous system regulation. Here's how:
Sympathetic and Parasympathetic Balance:
The autonomic nervous system is divided into the sympathetic nervous system (SNS), which controls the body's "fight-or-flight" responses, and the parasympathetic nervous system (PNS), responsible for "rest-and-digest" functions. A well-regulated nervous system ensures that the body can properly switch between these two states, promoting both acute stress management and long-term recovery.
- Sympathetic overactivation (chronic stress) is associated with increased wear and tear on the body, contributing to conditions such as cardiovascular disease, metabolic dysfunction, and chronic inflammation, which can shorten lifespan.
The parasympathetic nervous system, on the other hand, promotes healing, repair, and energy conservation. It reduces the effects of chronic stress and enhances processes like cellular regeneration and immune function, which are essential for longevity (Thayer et al., 2009).
Reduction of Chronic Inflammation:
Chronic low-grade inflammation is a key factor in aging and is linked to diseases such as diabetes, atherosclerosis, cancer, and neurodegenerative disorders. Nervous system regulation, particularly through the vagus nerve (a major component of the PNS), helps modulate the body’s inflammatory response. The vagus nerve plays a significant role in the inflammatory reflex, which reduces the production of pro-inflammatory cytokines, protecting the body from excessive inflammation that accelerates aging (Tracey, 2002).
Proper nervous system regulation limits the long-term damage caused by inflammation, which supports healthy aging and increases longevity by protecting tissues, organs, and cells from chronic stress.
Heart Rate Variability (HRV) as a Marker of Longevity:
Heart rate variability (HRV) is a key indicator of autonomic nervous system balance. High HRV is linked to better cardiovascular health, greater stress resilience, and longer lifespan. HRV reflects the balance between sympathetic and parasympathetic activity, with higher HRV indicating better regulation and flexibility of the nervous system.
Individuals with high HRV tend to have lower risks of developing age-related diseases, including heart disease and diabetes, as it suggests efficient nervous system regulation and better recovery from stress (Thayer et al., 2009). In contrast, low HRV is associated with chronic stress, poor recovery, and a higher risk of mortality, as it reflects persistent sympathetic dominance and reduced parasympathetic activity.
Stress Management and Longevity:
Chronic stress is one of the leading factors that reduce longevity, primarily due to its harmful effects on cellular aging. Stress activates the sympathetic nervous system, leading to the release of cortisol and norepinephrine. Over time, chronic stress and elevated cortisol levels can lead to the shortening of telomeres, the protective caps on chromosomes that are markers of biological aging.
- Shorter telomeres are associated with an increased risk of age-related diseases and premature death.
Proper nervous system regulation, particularly through the activation of the parasympathetic nervous system, helps manage stress and protect telomeres from damage, promoting cellular health and longevity (Epel et al., 2009).
Impact on Sleep and Regeneration:
Sleep is essential for both physical and mental recovery and plays a key role in longevity. A well-regulated nervous system, especially the parasympathetic branch, supports deep, restorative sleep, which is when the body engages in critical processes such as muscle repair, immune function, and memory consolidation.
- Lack of sleep or poor sleep quality, often caused by nervous system dysregulation (such as chronic sympathetic overactivity), is associated with accelerated aging, cognitive decline, and an increased risk of chronic diseases (Walker, 2017).
Proper nervous system regulation enhances sleep quality, which in turn supports cellular regeneration, reduces oxidative stress, and improves overall health, all of which are important for longevity.
Enhanced Immune Function:
A well-regulated nervous system promotes healthy immune function, helping the body defend against infections, repair damaged tissues, and maintain overall vitality. The vagus nerve plays a key role in modulating immune responses through its anti-inflammatory effects, which helps prevent the immune system from becoming overactive and damaging healthy cells, a process that contributes to aging.
Nervous system dysregulation, particularly persistent sympathetic activation, can suppress immune function, making the body more vulnerable to infections, cancers, and autoimmune disorders. Proper parasympathetic activation supports a balanced immune response, which is crucial for longevity (Tracey, 2002).
Cognitive Health and Longevity:
Cognitive decline, including conditions such as Alzheimer’s disease and dementia, is a major concern in aging. The nervous system, particularly the parasympathetic nervous system, influences cognitive function by regulating neuroplasticity, memory consolidation, and emotional regulation.
- Regular activation of the parasympathetic system (through activities such as mindfulness, meditation, or controlled breathing) supports brain health, reduces the risk of cognitive decline, and enhances emotional resilience, all of which are linked to longer lifespan.
Conversely, chronic stress and dysregulated sympathetic activity increase the risk of cognitive decline, primarily through the damaging effects of prolonged cortisol exposure on the hippocampus, a brain region crucial for memory (McEwen & Gianaros, 2011).
Conclusion:
A well-regulated nervous system promotes longevity by balancing the body's stress responses and restorative processes. Proper regulation of the autonomic nervous system, particularly through parasympathetic activation, reduces inflammation, supports cardiovascular health, enhances sleep quality, preserves immune function, and protects cognitive health. Conversely, chronic stress and nervous system dysregulation accelerate the aging process, increasing the risk of chronic diseases and reducing lifespan.

Conclusion
A well-regulated nervous system is crucial for maintaining balance in stress responses, recovery, energy management, and long-term health. Through its innovative use of Pulsed Pressure Waves, Shiftwave helps users achieve optimal autonomic balance by modulating sympathetic and parasympathetic nervous system activity. The effects of this modulation, as measured by EDA and HRV, lead to improvements in sleep quality, focus, energy, pain management, recovery, and longevity. Shiftwave offers a scientifically validated tool for enhancing autonomic nervous system resilience and overall well-being.

References
- Boucsein, W. (2012). Electrodermal Activity. Springer Science & Business Media.
- Thayer, J. F., Åhs, F., Fredrikson, M., Sollers III, J. J., & Wager, T. D. (2010). "A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health." Neuroscience & Biobehavioral Reviews.
- McEwen, B. S. (2007). "Physiology and neurobiology of stress and adaptation: Central role of the brain." Physiological Reviews.
- Lombardi, C., Pengo, M. F., & Parati, G. (2019). "Obstructive sleep apnea syndrome and autonomic dysfunction." Autonomic Neuroscience.
- Epel, E. S., et al. (2009). "Accelerated telomere shortening in response to life stress." PNAS.
- Woolf, C. J. (2011). "Central sensitization: Implications for the diagnosis and treatment of pain." Pain.
- Martucci, K. T., et al. (2019). "Pain and the autonomic nervous system: Clinical and experimental research." Neuroscience.
- Arnsten, A. F. T. (2009). "Stress signaling pathways that impair prefrontal cortex structure and function." Nature Reviews Neuroscience.
- Kadoya, M., & Koyama, H. (2019). "Sleep, autonomic nervous function and atherosclerosis." International Journal of Molecular Sciences. Link to PDF
- Lombardi, C., Pengo, M. F., & Parati, G. (2019). "Obstructive sleep apnea syndrome and autonomic dysfunction." Autonomic Neuroscience. Link to Article
- Meerlo, P., Sgoifo, A., & Suchecki, D. (2008). "Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems, and stress responsivity." Sleep Medicine Reviews. PDF
- McKnight, C., Carlson, B. E., Madadi, M. Y., Simon, M. J., & Iliff, J. J. (2020). “New insights into cerebrospinal fluid regulation of neuroinflammation and neurodegeneration.” Nature Neuroscience.
- Moldofsky, H., & Luk, W. P. (2002). "Sleep Regulation and the Autonomic Nervous System." Taylor & Francis. Link to Chapter
- Picchioni, D., Duyn, J. H., & Horovitz, S. G. (2021). “Autonomic arousals in sleep contribute to brain fluid pulsations.” Science Advances.
- Simon, M. J., & Iliff, J. J. (2016). “Perivascular pathways in the brain: Role of the glymphatic system in neuroinflammation and neurodegenerative diseases.” Cell Metabolism.
- Wang, Z., Tsai, H. H., & Yu, X. (2022). “Autonomic regulation of cerebrospinal fluid dynamics.” Journal of Cerebrovascular Research.
- McEwen, B. S. (2007). “Physiology and neurobiology of stress and adaptation: Central role of the brain.” Physiological Reviews.
- Thayer, J. F., Åhs, F., Fredrikson, M., Sollers III, J. J., & Wager, T. D. (2009). “A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health.” Neuroscience & Biobehavioral Reviews.
- Arnsten, A. F. T. (2009). “Stress signaling pathways that impair prefrontal cortex structure and function.” Nature Reviews Neuroscience.
- Arnsten, A. F. T. (2009). "Stress signaling pathways that impair prefrontal cortex structure and function." Nature Reviews Neuroscience. Link to article
- Thayer, J. F., Åhs, F., Fredrikson, M., Sollers III, J. J., & Wager, T. D. (2009). "A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health." Neuroscience & Biobehavioral Reviews. Link to PubMed
- McEwen, B. S. (2007). "Physiology and neurobiology of stress and adaptation: Central role of the brain." Physiological Reviews. Link to PubMed
*20, 21, 22 - These references highlight how the balance between the sympathetic and parasympathetic systems plays a critical role in enhancing or hindering focus. - McEwen, B. S. (2007). "Physiology and neurobiology of stress and adaptation: Central role of the brain." Physiological Reviews. Link to PubMed
- Thayer, J. F., Åhs, F., Fredrikson, M., Sollers III, J. J., & Wager, T. D. (2009). "A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health." Neuroscience & Biobehavioral Reviews. Link to PubMed
- McEwen, B. S., & Wingfield, J. C. (2003). "The concept of allostasis in biology and biomedicine." Hormones and Behavior. Link to PubMed
- Arnsten, A. F. T. (2009). "Stress signaling pathways that impair prefrontal cortex structure and function." Nature Reviews Neuroscience. Link to article
*23, 24, 25, 26 - These references illustrate the connection between a well-regulated nervous system and sustained energy and vitality, both physically and mentally. - Woolf, C. J. (2011). "Central sensitization: Implications for the diagnosis and treatment of pain." Pain. Link to PubMed
- Martucci, K. T., et al. (2019). "Pain and the autonomic nervous system: Clinical and experimental research." Neuroscience. Link to PubMed
- Tracey, K. J. (2002). "The inflammatory reflex." Nature. Link to PubMed
- Callaghan, B. C., Cheng, H. T., Stables, C. L., Smith, A. L., & Feldman, E. L. (2012). "Diabetic neuropathy: Clinical manifestations and current treatments." The Lancet Neurology. Link to PubMed
- Baron, R. (2006). "Mechanisms of disease: Neuropathic pain—a clinical perspective." Nature Clinical Practice Neurology. Link to PubMed
- Ji, R. R., Nackley, A., Huh, Y., Terrando, N., & Maixner, W. (2014). "Neuroinflammation and central sensitization in chronic pain." Journal of Neuroinflammation. Link to PubMed
- McEwen, B. S. (2007). "Physiology and neurobiology of stress and adaptation: Central role of the brain." Physiological Reviews. Link to PubMed
*27, 28, 29, 30, 31, 32, 33 - These references highlight the interaction between nervous system regulation, pain management, and the development of neuropathy. Proper regulation can mitigate pain, while dysregulation can worsen pain and lead to neuropathic complications. - McEwen, B. S. (2007). "Physiology and neurobiology of stress and adaptation: Central role of the brain." Physiological Reviews. Link to PubMed
- Porges, S. W. (2011). "The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation." W. W. Norton & Company. Link to PubMed
- Thayer, J. F., Åhs, F., Fredrikson, M., Sollers III, J. J., & Wager, T. D. (2009). "A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health." Neuroscience & Biobehavioral Reviews. Link to PubMed
- Sapolsky, R. M., Romero, L. M., & Munck, A. U. (2000). "How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions." Endocrine Reviews. Link to PubMed
- Walker, M. P. (2017). "The role of sleep in cognition and emotion." Annals of the New York Academy of Sciences. Link to NIH
*34, 35, 36, 37, 38 - These references highlight the critical role of nervous system regulation in facilitating both mental and physical recovery, emphasizing the balance between stress responses and restorative processes. - Thayer, J. F., Åhs, F., Fredrikson, M., Sollers III, J. J., & Wager, T. D. (2009). "A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health." Neuroscience & Biobehavioral Reviews. Link to PubMed
- Tracey, K. J. (2002). "The inflammatory reflex." Nature. Link to PubMed
- Epel, E. S., et al. (2009). "Accelerated telomere shortening in response to life stress." PNAS. Link to PubMed
- Walker, M. P. (2017). "The role of sleep in cognition and emotion." Annals of the New York Academy of Sciences. Link to NIH
- McEwen, B. S., & Gianaros, P. J. (2011). "Stress- and allostasis-induced brain plasticity." Annual Review of Medicine. Link to PubMed
*39, 40, 41, 42, 43 - These references provide evidence on how the regulation of the nervous system influences longevity by affecting stress management, inflammation control, immune function, and overall health.